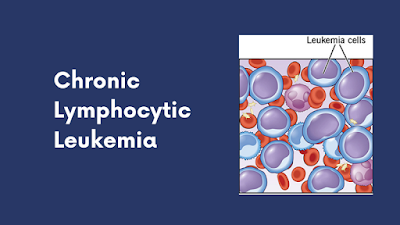
Recent stats suggest that out of the total number of Leukemia cases, Chronic Lymphocytic Leukemia or CLL will account for a quarter of it. Most people with this condition live up to 10-20 years after getting diagnosed and getting proper treatment. However, there are some cases where disease progression is rapid, and the patients live only up to a few years.
Causes of CLL:
It usually starts due to a certain genetic mutation in the blood-producing cells that leads to the production of ineffective and abnormal lymphocytes. Unlike normal lymphocytes, they don’t die. Instead, they continue multiplying and starts accumulating in the blood and specific organs gradually, which causes complication. The process also interferes with the healthy cells in the bone marrow, and as a result, the production of normal blood cells gets affected.
The risk factors may include exposure to certain chemicals like herbicides and insecticides. Having a family history of blood or bone marrow cancer may increase your chances too.
Symptoms
- Swollen glands in the armpits, neck, and groin
- Unusual bruising and bleeding often
- Night sweats
- Shortness of breath and pale skin
- Anaemia
- Unusual weight loss
These are some of the recognizable symptoms. If you face any of these, it is recommended to contact your healthcare professional and get a checkup done.
Relation between Chronic Lymphocytic Leukemia and Myeloma
Both the conditions—Multiple Myeloma and CLL consist of overlapping epidemiologic features. Even though they are seen to be originating from the mature B cells, the chances of these two cases coinciding are quite rare. In Multiple Myeloma, the plasma cells are affected, whereas, in CLL, the lymph nodes, liver and spleen are affected, which ultimately causes the bone marrow to stop functioning.
Although both CLL and Myeloma are blood cancers, the latter is formed in the bone marrow and responsible for the subset of WBC to form a distinctive protein that causes cancer to grow and spread. They have parallel as well as divergent features.
The common features include stage-dependent anaemia and immunodeficiency. Not only that, but both diseases respond to alkylating agents.
Treatment of Chronic Lymphocytic Leukemia
Although there are different options available, one must also have to keep in mind that there are side effects of each one of them. The upsides and downsides are measured with respect to various medical tests conducted, and then the doctor prescribes which way to go.
1. Radiation Therapy
If the condition has been diagnosed in a localized stage and the only thing to deal with is an enlarged spleen or swollen lymph nodes, you can opt for low-dose radiation therapy. This treatment of Leukemia is safe and shows much lesser side effects.
2. Surgery
Also referred to as Splenectomy, one may go with this option to remove the enlarged spleen. However, this is not advisable for an advanced stage condition.
3. Stem Cell Transplant
If it is a high-risk condition, stem cell transplant could be considered as an option for early treatment.
4. Drug Therapy: Chemo and Targeted
Chemotherapy and targeted therapy are two of the most commonly approached treatment options. The drugs can either be prescribed alone or in combination with other medications to yield the best results. Mention may be made of the following drugs in this respect:
Ibrutinib: It is classified as a Bruton’s Tyrosine Kinase that can inhibit the B-cell lymphoma 2 protein. It is prescribed alone or in combination with Rituximab. The typical dosage for this condition is 420mg per day, i.e., three Ibrutinib 140 mg tablets per day. However, it may be decreased depending upon the extent of the condition and response from the body.
Alemtuzumab: It has been approved as both first-line and second-line treatment for Chronic Lymphocytic Leukemia. The drug is administered into the body as an injection in the vein. Doctors can prescribe it alone or with Rituximab. This targeted cancer drug can be classified as a monoclonal antibody.
Venetoclax: It is a B-cell Lymphoma-2 oral inhibitor that is prescribed as a targeted drug alone or in combination with Obinutuzumab and Rituximab. High-risk older patients may also benefit from the combination of Venetoclax and Ibrutinib. The starting dose is 20mg daily for a week, which then ramps up to Venetoclax 100 mg to 400mg per day. The average treatment time is 24 months.
Obinutuzumab: This is an antineoplastic cytotoxic drug that acts as an anti CD20 monoclonal antibody. It is a chemotherapy drug that is given to the patient as an intravenous infusion through a dedicated line. The B cells have CD20 proteins with which the drug binds to destroy them by engaging the adaptive immune system.
These are some of the medications that have shown to slow down disease progression in CLL patients and helped to increase the survival rate over the years. Even though there are side effects to this, they are not consistent and easily manageable.
Conclusion
Typically, out of 10, 7 patients suffering from CLL have a survival rate of 5 years or more after getting diagnosed. The length of survival time also depends on your overall health condition, medical history and the extent of the disease. If the diagnosed patient has been in a healthy condition for most of their lives, the chances of survival are more for them. The treatment options do not guarantee a surefire cure; they are only for managing the condition and treating the symptoms so that they don’t get worse over time.
Read:- Venetoclax for Chronic Lymphocytic Leukemia